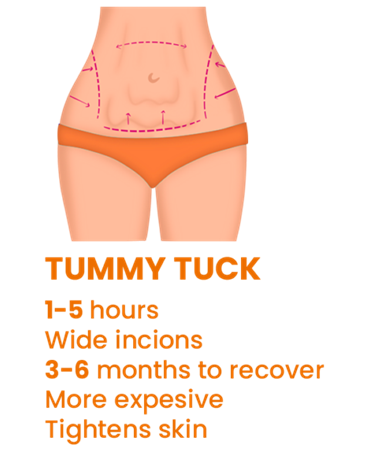
Weight loss helps address health issues like the risk of congenital conditions and can boost self-esteem due to body contouring. The loss, however, can result in loose and sagging skin that does not respond to exercise, and may require removal through surgery to enhance the contouring further. Two primary surgical options exist – panniculectomy and tummy tuck. The choice between the two may be confusing. Though the end goal remains the same, there are differences in the process, candidates, cost, and risks. A panniculectomy involves removing the panniculus, the excess loose skin that forms a flap below the waistline and over the thighs. The panniculus does not emanate from pregnancy, excess weight, or regular weight loss. It emanates from losing excess body weight, typically over 100 pounds, mostly from extensive weight loss procedures like gastric bypass. The extent of a panniculectomy, considered a medical procedure, depends on how much skin is removed. A tummy tuck, on the other hand, is considered a cosmetic procedure that involves removing excess stomach skin and tightening the abdominal muscles. Sometimes surgeons add an abdominal mesh to reinforce muscle repair. This woven mesh surgically temporarily or permanently supports organs after surgery or damaged tissue during healing. The second difference between a panniculectomy and a tummy tuck is eligibility. The former is best for patients with life-impacting sagging skin, which follows heavy weight loss, especially gastric bypass. Other candidates include individuals experiencing hygiene issues under the skin such as ulcers and infections, especially below the pubic region. The excess skin flap can also affect the individual’s mobility. On the other hand, a tummy tuck addresses sagging skin that does not affect the individual’s health and is mainly for cosmetic purposes, especially contouring the body for a more hourglass shape. Other good fits include individuals with sagging skin following a pregnancy who cannot get rid of the excess skin despite exercise and diet changes. In conjunction with liposuction, a tummy tuck can help resolve body-related self-esteem issues and those seeking to get rid of more skin after a panniculectomy. The third difference is the recovery time after each procedure. Recovery from any mild to major surgery involves surgical drains, skin glue, steri-strips, and the dressing. The surgeon provides instructions on how to care for each over the recovery period. A panniculectomy typically takes eight weeks to heal. However, the time may vary depending on the surgery’s extent and the patient’s attendance to the wound after the surgery, especially daily tasks and nutrition. Even weeks after the healing has taken place, however, the patient should refrain from strenuous activities like heavy lifting. Tummy tucks take less time to recover from due to less surgery complexity – usually four to six weeks. With proper care, especially hygiene of the surgical area, the patient should resume regular activity, including strenuous tasks, in the first few weeks following the procedure. Due to the extent of the surgery, panniculectomies are more costly than tummy tucks. A procedure typically costs between $8,000 and $15,000, plus additional fees like anesthesia, compared to an average of $6,000 for a tummy tuck. However, as a medical procedure, insurance companies may cover part or all of a panniculectomy. There is also the cost of taking time off work, especially for self-employed individuals – patients should set aside a minimum of eight weeks for recovery, compared to four to six weeks for a tummy tuck. Finally, the risks and side effects differ. Although both procedures cause discomfort and pain, the side effects tend to be more severe for panniculectomy. These can include pain post-surgery, fluid retention, and numbness. Other effects, though rare, include chest pain, heart palpitations, shortness of breath, and infections. Conversely, tummy tuck patients may experience bruising, numbness, deep vein thrombosis, and bleeding around the surgical area.
Karim Sarhane, MD