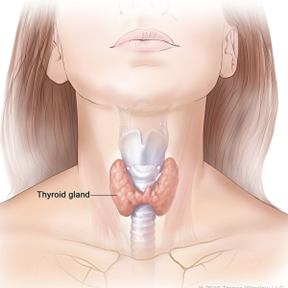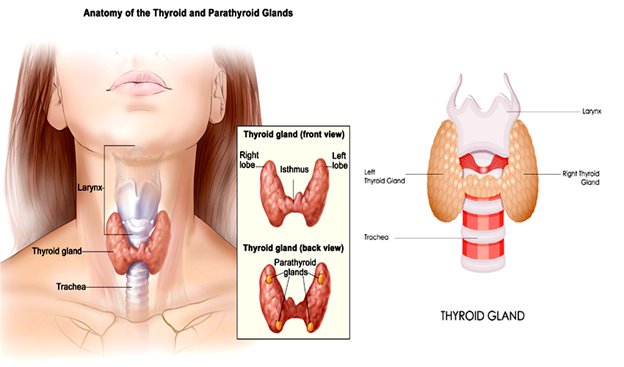
Thyroid cancer is a condition where malignancy grows in the thyroid gland. The thyroid gland is a butterfly-shaped organ that sits at the base of the trachea (windpipe) and has a right and left lobe. A thin body of tissue called the isthmus connects these lobes. Malignancy is a condition where cell division occurs abnormally and may invade and infect nearby cells. The thyroid gland uses iodine to synthesize several essential hormones, including triiodothyronine, tetraiodothyronine, and calcitonin. These hormones control and regulate various physiological functions such as body weight, heart rate, blood pressure, and body temperature. Within the thyroid gland, there may be nodules. A doctor may discover these abnormally grown thyroid gland cells during a patient’s check-up. These nodules may be solid or filled with liquid. Over 90 percent of these nodules are benign, while 10 percent are malignant. Initially, thyroid cancer may not exhibit symptoms. However, as the malignant cells invade more nearby cells, signs and symptoms will eventually appear. The most common of these include neck swelling, difficulty swallowing food and breathing, and voice changes. As a result, healthcare professionals recommend regular check-ups due to the silent nature of the condition’s onset. About 53,000 Americans get thyroid cancer treatment yearly. While most treatments are successful, around 2,000 patients die annually due to the disease. Women are at three times the risk of getting thyroid cancer than men. For women, most cases involve those between 40 and 50 years old, while in men, most of those affected are from 60 to 70 years old. The condition may also affect children, but only in rare cases. The condition’s risk factors include a diet low in iodine, gene mutations, a family history of the disease, an enlarged thyroid (also known as goiter), and obesity. Other risk factors are radiation therapy in the head and neck, especially for children, and exposure to radioactivity, such as that experienced during a nuclear power plant accident. There are different types of thyroid cancer, including anaplastic, follicular, medullary, and papillary. Accounting for about 2 percent of all thyroid cancer types, anaplastic thyroid cancer, though rare, is the hardest to treat. The malignant cells grow quickly and may spread to surrounding tissues and other parts of the body. Medullary thyroid cancer also accounts for around 2 percent of all cases. It is caused by a genetic mutation leading to a faulty gene. As a result, this condition is primarily hereditary, with a quarter of those infected having a family history of the disease. Similar to anaplastic thyroid cancer, follicular thyroid cancer is metastatic. This is a condition where the cancer cells spread from the original tumor and enter the lymphatic system or bloodstream, infecting other body parts. Follicular thyroid cancer is also hard to treat, since it may spread to the bones and organs such as the lungs. It accounts for about 15 percent of all cases. Diagnosis for thyroid cancer may be through blood tests, biopsy, radioiodine scans, and imaging scans. Blood tests check whether the thyroid is functioning properly and hormone levels. A biopsy involves removing the suspect tissue and observing it in a laboratory for cancer cells. Radioiodine scans involve a patient swallowing a safe amount of radioactive iodine and using a special device to measure radioactivity in the thyroid gland. The areas that emit less radioactivity require more testing to ascertain if there is cancer. Last, imaging diagnosis techniques, including computed tomography (CT) scans and positron emission tomography (PET) scans, can be used to detect cancerous growths. Treatment depends on the tumor’s size and if it has spread. Common treatment methods include chemotherapy, hormone therapy, radiation therapy, radioiodine therapy, and surgery. Chemotherapy involves administering drugs to the patient that kill the cancerous cells. Hormone therapy stops the release of hormones that spread cancer or may cause it to recur. With radiation therapy, a machine emits targeted radiation that only kills the cancerous cells, while in radioiodine therapy, the patient takes a higher dose of radioactive iodine than that used in radioiodine scans to shrink and destroy the cancerous cells. Last, surgery involves physically removing the tumor. The surgeon may perform lobectomy, where they remove part of the thyroid gland, or thyroidectomy, where they remove all of the thyroid gland.
Karim Sarhane, MD